Modern Healthcare
NEW YORK – Four months since the first COVID-19 case was reported in the U.S., the demand for testing for the SARS-CoV-2 virus still far outpaces the supply, even as test developers scramble to increase their testing capacity and new types of tests make their way into the market.
Despite assurances early on from President Trump that everyone who needed a test would get one, and his more recent claim that the U.S. has tested more people than all other countries combined — an assertion that has been disproven — the reality is that very few Americans have gotten tested, including many who may have been infected with the SARS-CoV-2 virus.
According to the COVID Tracking Project, about 8.4 million Americans, or 2.5% of the total U.S. population, were tested for COVID-19 as of May 9. Meanwhile, dozens of tests have been authorized by the Food and Drug Administration for emergency use, with the list growing almost daily. Along with molecular tests, serology tests, and most recently, a rapid, protein-based antigen assay, have also been authorized for use to help diagnose COVID-19 and track spread of the disease.
Although experts say testing is crucial to reopening the economy, the U.S. testing pipeline faced early problems. While the situation is improving, the country still has not caught up.
With a few months left until a second wave of coronavirus infections is expected in the fall, that could leave the U.S. once again unprepared and vulnerable.
Early problems
On Jan. 31, a little more than two weeks after COVID-19 hit the U.S., the Trump administration declared a public health emergency. Four days later, the FDA gave a Centers for Disease Control and Prevention test an emergency use authorization.
But the U.S. was already playing from behind, according to many experts.
“We fell behind the curve from the beginning,” said Harry Glorikian a general partner at New Ventures Funds, a venture capital firm that invests in therapeutics, precision medicine, diagnostics and technology companies.
In particular, he noted that aside from the CDC, only diagnostic test makers were initially allowed to develop tests for the coronavirus, while public health laboratories were not. Amid pressure from laboratory organizations and facing the wildfire spread of COVID-19 — as well as problems with CDC’s test — the FDA later changed its policy and allowed high-complexity, CLIA-certified labs to develop their own assays.
By then, the demand for tests already outweighed the supply and that hampered clinicains ability to identify and isolate patients, Glorikian said.
In a research note, Jack Meehan, an analyst formerly at Barclays, also noted that “testing capacity at the onset of the COVID-19 outbreak was clearly insufficient” and the limited testing options meant public health officials couldn’t contain the disease’s spread.
The CDC’s test was quickly followed by others, many of which used PCR to detect viral nucleic acid. Later approved tests included antibody-based serology tests. There are currently 70 FDA-authorized tests on the market and another two dozen molecular-base laboratory-developed tests also have EUAs. The latter can be used only in the labs that developed them.
The tests have come to market even faster than past public health emergencies, including the Ebola crisis and Zika virus outbreak. Normally, it would take a year, or longer, to get a new assay into the market, but during the pandemic, that timeline shrank to a few short weeks, Scott Whitaker, president and CEO of AdvaMed, a medical device trade association, said during a press conference in late April.
The COVID-19 pandemic represents “the first time that diagnostic companies and labs have had to deal with a pandemic on such a broad geographic scale,” according to Davide Manissero, chief medical officer at Qiagen.
“Since the discovery of molecular technology, we have never seen such an increase in demand for our products in such a short period of time,” he said Davide Manissero.
That has forced test developers to work overtime, and the number of tests they say they are producing is staggering. Roche, the first commercial developer to receive EUA for a SARS-CoV-2 test, currently provides 15 million tests per month.
Meanwhile, Danaher’s Cepheid has shipped 2 million cartridges for its SARS-CoV-2 test, which received EUA at the end of March, and it expects to ship 6 million per quarter, Danaher President and CEO Thomas Joyce said during the company’s first quarter conference call last week.
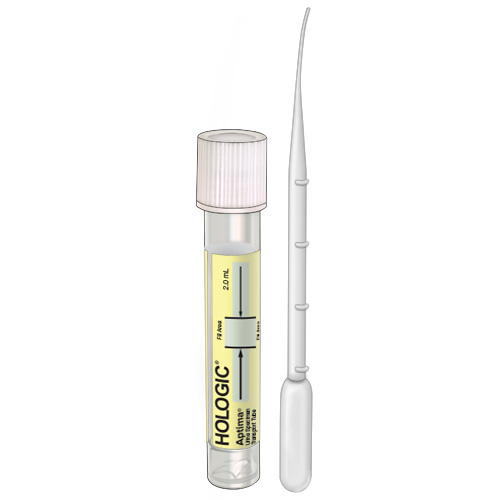
Hologic President, Chairman, and CEO Stephen MacMillan said during his firm’s fiscal second quarter conference call in April that in a one-week period, would provide 3 million tests leveraging the firm’s Aptima technology, and starting in late May, it would produce at least 1 million COVID-19 tests per week.
The firm also said it is now producing almost 600,000 of the SARS-CoV-2 assays for its Panther Fusion system per month, representing a twelvefold increase in the company’s prior capacity for tests that run on the platform.
Addtionally, in April, Luminex said it would ship between 300,000 and 500,000 of its COVID-19 tests. It is not disclosing exact numbers but said that it has received orders for “hundreds of thousands of tests, ” with demand exceeding expectations.
Becton Dickinson, which offers two molecular assays and an antibody assay for the coronavirus, said it is selling 50,000 COVID-19 tests per week.
It is unclear how many of the tests being sold by the companies are for use in the U.S.
On the laboratory side, the American Clinical Laboratory Association said its members have performed 3.48 million tests as of April 29. ACLA represents many of the major reference labs, including Quest Diagnostics, Laboratory Corporation of America, and Opko Health’s BioReference Laboratories.
Quest recently said that it has reported the results of approximately 1.5 million COVID-19 molecular diagnostic tests since it introduced testing services on March 9. The lab company added that it has the capability to perform approximately 50,000 of these diagnostic tests per day, or approximately 350,000 tests per week. It is using three different molecular tests in 12 of its U.S. labs.
It has also reported results of approximately 325,000 COVID-19 antibody tests as of early May, and it is performing about 150,000 antibody tests a day or about 1 million a week.
Even with the current supply and plans to further ramp up the testing pipeline, some diagnostics firms have expressed reservations that they can meet demand. In a research note published in late April, Doug Schenkel, a financial analyst at Cowen, said that between 45 million and 85 million molecular SARS-CoV-2 tests could be needed in the U.S. and Europe through August 4.
“While this is a big number, we note that it plausibly could be low because it does not fully contemplate the need for repeat testing of those that test positive, nor does it include the use of these tests in other areas,” such as using them to clear individuals for elective procedures.
Moving into the fall and the flu season, the need for molecular SARS-CoV-2 tests could reach 20 million. “When we include potential applications such as healthcare workers, surgical screening, and others, there is a potential need for 100 million to 200 million just in the U.S. over the balance of this year,” Schenkel wrote.
The industry is not equipped to churn out such massive numbers of tests. Abbott Laboratories, which currently has three approved tests, noted on its first-quarter earnings call in mid-April that increasing manufacturing has been difficult. CEO Robert Ford said on the call that Abbott had the capacity to produce 4 million antibody and PCR tests and 50,000 rapid point of care tests in the month of April. Since then, the firm said that it could manufacture 2 million point of care tests per month in June.
But that’s still not enough tests to keep up with the demand, Ford said, adding that while Abbott is scaling up manufacturing, it will take time.
Similarly, since Mesa Biotech’s 30-minute PCR point-of-care assay received EUA from the FDA in March, the company has been “overwhelmed by interest” in the test, CEO Ingo Chakravarty said in an interview, adding the focus right now is scaling up manufacturing and increasing manufacturing lines.
He said Mesa is getting “creative” with manufacturing lines due to social distancing protocols and is renting any available space near its office to increase manufacturing capability. Mesa provided 20,000 tests to its distributor, some of which are being used to validate the test, and Chakravarty said the company has received 1,500 inquiries domestically and internationally about the test.
Mesa is also increasing automation and hiring additional employees, as well as speeding up onboarding processes, to ensure it has enough employees and manufacturing capability to meet demand.
Other firms have also found the need to beef up their staff, including Avellino Lab, whose PCR-based test received EUA in March. Eric Bernabei, the company’s chief sales and marketing officer, said Avellino has quadrupled its staff and switched to a three-shift schedule to meet the demand for testing, which is outstripping supply. Bernabei added that Avellino had the capacity to provide 20,000 tests in April and were aiming to reach 120,000 to 150,000 tests in May and 200,000 in June.
But finding and hiring qualified personnel has been a challenge for many labs. “Trained lab personnel … are not falling from the proverbial tree,” New Ventures Funds’ Glorikian said.
MacMillan echoed his sentiment and said on Hologic’s Q2 call that many investors have been asking why U.S. testing volumes are still limited although the diagnostics industry is producing more tests.
“One reason is that many of these tests are run on manual or semi-automated systems, putting a tremendous strain on lab technicians who are in short supply to begin with.”
Short on supplies
Test makers are also facing shortages of reagents, swabs, and various collection devices.
American Association for Clinical Chemistry President Carmen Wiley said in an interview that supply issues were a major problem for AACC members, and some labs have started validating alternate transport media and are using 3-D printers to manufacture nasopharyngeal collection swabs.
Since many test kits are being allocated based on perceived need, some labs have the capacity to run more tests but simply don’t have the reagent kits. She noted that there are labs with the capacity to run 1,300 tests per day but have only received 800 kits from the manufacturers.
Jordan Laser, chair of the Association for Molecular Pathology’s professional relations committee, said in an interview that the “entire global supply chain is strained right now due to both an overwhelming demand for materials and required diagnostic testing capacity around the world. This includes the RNA extraction kits, primers, probes, and enzymes, as well as the physical sample collection materials — swabs and containers for storage and transportation.”
According to a recent survey conducted by AMP, more than 70% of respondents said they experienced supply chain interruptions, resulting in testing delays and reduced testing capacity. Smaller labs also reported favoritism in who are getting supplies: 60% of respondents reported that some of the government’s supplies and reagents are being allocated to the larger reference laboratories, said Laser who is also medical director of Long Island Jewish Medical Center, Pathology and Laboratory Medicine.
Like test developers, reagent producers are trying their best to increase the supply. Qiagen has historically allocated global production capacity to manufacture RNA nucleic extraction reagents to supply about 1.5 million patient tests monthly, Manissero said. But in the midst of the pandemic the firm anticipates ramping production capacity for its extraction reagents to support testing for more than 6.5 million patients per month as of the end of April. It further expects increasing capacity to support more than 10 million patient tests per month by the end of June and more than 20 million tests per month by the end of 2020.
The firm noted that a capacity expansion project is underway at sites in Europe and the U.S., and to help meet testing demand, it has hired additional staff, moved to three shifts working around the clock, and switched to larger kit sizes.
Robert Boorstein, medical director for oncology and esoteric testing at Brooklyn-based Lenco Diagnostic Laboratories, said that he believes that “manufacturers are still not producing as much reagent as all their customers say they need.”
The shortage of test collection devices, he added, has become “a big problem across the board and is hampering large test suppliers with respect to their abilities to ramp up and produce the number of tests they want to produce.”
Some diagnostic test suppliers have deliberately stopped testing for certain diseases, for example, to enable them to allocate more resources to manufacturing and supplying COVID-19 tests.
While some companies are having trouble sourcing reagents, others are probably having trouble sourcing plastics for test cartridges. “The conditions and challenges are not the same at Roche as they are at Abbott or Hologic,” Boorstein said.
In January in anticipation of a spike in coronavirus testing, Luminex engaged with its supply chain customers and began adding critical components to its inventory. Longstanding relationships with suppliers enabled it to obtain testing supplies and other products in competition with other companies. As a result, the molecular diagnostics firm has been able to increase its capacity to manufacture its SARS-CoV-2 molecular tests by 400% since the beginning of January, Mark Hunter, senior director of global supply chain at Luminex, said.
Still, the Austin, Texas-based firm has not been immune to difficulties created by the shortage in supplies.
“Though we were able to quickly get to the level of capacity for which we had been planning this year, we have begun to run into constraints that prevent U.S. from expanding beyond a certain point,” Hunter said. “We know that if we could build more tests, we would sell them.”
Not sick enough
Aside from supply shortages, others also pointed to another culprit why more Americans are not getting tested: they are essentially too healthy.
“Guidelines stipulating who can get tested are now the greatest barrier to broader testing,” said Kyle Fetter executive vice president and general manager of diagnostic services at revenue cycle management and lab informatics firm Xifin.
“A patient has to be perfectly symptomatic to get a test from a lot of the labs that have capacity. When we talked to our labs about that, they said state departments of health are driving guidelines that are preventing more tests from being ordered,” he said in an interview.
Hologic’s MacMillan added that states, hospitals, and doctors “have been fairly restrictive in allowing people to get tested,” and people have had to jump through hoops to get a test “because the supply was so constrained.
“As people become more comfortable that the supply is really starting to ramp up, I think we will start to see … more of the loosening of the gauntlet that a patient has to run through to get tested,” he added.
That may already be happening, according to Emily Volk, president-elect of the College of American Pathologists. “In the beginning we saw strict adherence to travel history, upper respiratory symptoms, and fever for people allowed to get testing,” she said in an interview. “Once it became clear we had community transmission, travel history no longer was necessary, for example.”
The “constellation of symptoms” for COVID-19 disease has also evolved to now include “a variety of gastrointestinal issues, malaise, and fatigue. And there are early reports of neurological and dermatological symptoms, including so-called COVID toes,” she said.
“As testing capabilities have grown and our understanding of the disease has expanded, we are seeing a lot more people being tested,” Volk said. “I hope the [IVD] industry can catch up and then keep up with the continued demand for testing of the broader population, including asymptomatic people in the community for epidemiological surveys.”
For more testing to occur, though, widespread use of coronavirus serology tests will need to happen, most experts agree. Unlike molecular tests, which detect active SARS-CoV-2 infection, serology tests detect antibodies to the coronavirus, and so are more suited for determining whether someone has been exposed to the virus. In particular, they can identify asymptomatic individuals who had the coronavirus.
Antibody tests have been seen as a tool for determining how widespread SARS-CoV-2 in in the population. For now, though, many are skeptical about them because of the less-than-optimal false positive and false negative rates for some of the tests.
“If you are receiving serology testing from a reputable diagnostic company, the performance characteristics are probably fine,” AACC’s Wiley said. “But until we have more information on that, I do think people need to be cautioU.S. on the interpretation of the serology tests.”
The FDA recently took note of such concerns and are now asking test developers to prove that their tests work. Originally, the agency allowed developers of such tests to market them without necessarily seeking an EUA. But last week, the agency said that test makers would need to provide validation that their products meet certain performance thresholds.
To date, 12 serology tests have received EUAs from the FDA for COVID-19 compared to 54 molecular tests, but the number of serology testing being done could explode. In addition to its authorized IgG test running on the Architect platform, Abbott on Monday received EUA for its IgG test for the Alinity I platform, and the firm said that it expects to ship almost 30 million antibody tests globally in May with capacity for 60 million tests in June.
Additionally, Siemens Healthineers said in an interview last week that it plans to launch a coronavirus antibody test by the end of May and plans to ship more than 25 million tests to run on the company’s Advia and Atellica immunoassay platforms.
When Roche received FDA EUA for its Elecsys Anti-SARS-CoV-2 antibody test last week, it said it would provide high double-digit millions of the test in May and would ramp up testing capacity moving forward.
Meanwhile, the new legislation called the Coronavirus Aid, Relief, and Economic Security Act, or CARES Act, provides $306 million to the National Cancer Institute specifically for the development of coronavirus serology tests.
More broadly, the legislation gives NCI $1.8 billion to develop new technologies for detecting SARS-CoV-2, and another $1 billion to the HHS’ Biomedical Advanced Research and Development Authority for R&D related to diagnostic, serology, or other SARS-CoV-2 tests or related supplies.
Another type of test, protein-based antigen tests, are also starting to gain visibility. Unlike PCR tests, which detect viral nucleic acid, rapid antigen tests detect viral proteins and can provide results more quickly than PCR tests, while being less expensive to manufactures, consumers, and insurers.
They are not a replacement for molecular tests because of sensitivity and specificity issues, but several firms are at work to develop more accurate rapid antigen tests, including heavy hitters such as Roche, Abbott, and Becton Dickinson. Avacta is also collaborating with Adeptrix to develop a high-throughput, mass spectrometry-based COVID-19 antigen test.
On Friday, a test from Quidel became the first rapid antigen test for SARS-CoV-2 to be issued EUA by the FDA.
In testimony to the Senate Help, Education, Labor, and Pensions Committee the same day, National Institutes of Health Director Francis Collins noted the institutes’ interest in developing such technology for COVID-19.
“One category [of testing] we will pursue actively is called viral antigen testing,” he said in his prepared remarks. “With time and effort, antigen tests can be modified to be done at home, which would allow for easier and more frequent testing.”
He also referred to the newly launched Rapid Acceleration of Diagnostics, or RADx, program, saying it could help developers overcome the sensitivity/specificity issues surrounding rapid antigen tests.
The FDA has also expressed interest in other testing technologies, including those that use alternative sample types to those typically use for PCR testing and antibody testing. Last month, the agency authorized a test from the Rutgers Clinical Genomics Laboratory originally developed by Thermo Fisher Scientific that was modified to use additional specimen types, such as saliva, to detect SARS-CoV-2. It was the first molecular COVID-19 test with EUA for use with saliva samples.
The EUA was amended last week to allow individuals to collect their own saliva samples and home to send to the Rutgers lab for testing. The FDA previously issued its first EUA for a coronavirus test with the option for the self-collection of patient samples to LabCorp on April 21.
Also last week, the FDA issued new guidelines to allow companies to develop and market tests with devices that allow individuals to swab their noses and mail them to labs to get tested for COVID-19, potentially opening up access to more and easier testing.
In the meantime, some say the demand for molecular testing for SARS-CoV-2 might be plateauing. Xifin’s Fetter said that U.S. labs are reporting that they now have capacity to run more COVID-19 tests than clinicians are ordering. The early delays in testing, shortages in reagents and swabs, and stringent rules that restricted who got tested are easing enough that “most labs are reporting having plenty of capacity,” he said.
Quest, LabCorp, and BioReference recently also reported their capacity for molecular testing were outpacing demand.
Regardless, no one — except perhaps Trump — is saying that coronavirus testing capacity is anywhere near where it needs to be, and in the fall, when the weather will cool, another tsunami of COVID-19 cases could strike.
Wiley said that no matter how many tests are manufactured, it still might not be enough. In a pandemic, more people keep getting sick, and demand keeps increasing at a faster pace than tests can be manufactured and delivered to the people doing the testing, creating a never-ending loop.
“By the time we get [tests] distributed throughout the United States and into labs, it still can’t meet the capacity we need,” she said.
An ACLA spokesperson added that labs may need to double or triple testing capacity to truly meet testing demands. In order to do that they “would need to invest in additional high-throughput testing platforms, train additional staff to perform testing and also maintain the necessary volume supplies.” Many companies are taking these measures, but the pandemic caught the country unaware and it is still trying to recover, she said.
Click here for original post on Modern Healthcare